Primary Care Review – August/September 2025
The 2026 CMS Proposed Physician Fee Schedule Rule: What’s In There for Primary Care and Population Health?
In a Nutshell
Every July, CMS releases a draft proposal describing the changes that they are proposing for the following year’s Physician Fee Schedule (PFS). After a comment period to collect public feedback, CMS finalizes the rule in November for implementation the following January. This year, there is plenty of good news for primary care. The proposed rule includes provisions that would lead to stronger investment in community-based primary care and better position Medicare to more effectively address chronic condition management and preventive care. Of all of the changes in the 1800 paged proposed rule, two stand out as key and CMS should be applauded for them and encouraged to finalize them. There is also one proposed change that would be transformative for primary care and population health if it were modified in the final rule. We’ve got some ideas on how that could be done. Read on!

First, let’s take a look at each of the two stand-out, policy-forward changes that we are excited about. The first is incorporating an “efficiency adjustment” that will improve the payment system by more fairly reimbursing cognitive work, the core of primary care.
The second is incorporating a site of service payment differential that would help to level the playing field for independent primary care practices. This change would decrease the financial incentive inherent in the current rule for health systems to purchase primary care practices and bill an additional facility fee for the same service in the same location as when the practice was independent.
There are also aspects of the proposed rule that if slightly modified, could be very promising. For example, CMS adds new Behavioral Health Integration (BHI) Add-On codes for the Advanced Primary Care Management (APCM) codes, bundles that encourage robust team-based care and improved outcomes for patients. CMS should be roundly congratulated for taking positive steps
forward to transition toward hybrid payment for primary care. But unless patient-cost sharing is waived for these codes, they will not be implemented. The great news is that CMS can do so and should be encouraged to do so in their final rule as there is a provision for cost-sharing to be waived for ‘personalized prevention care services’. The preponderance of APCM codes fit squarely under this was widely deployed. It is easy to submit comments to CMS to let them know how they can improve the proposed rule and at the end of The Detail section, we’ll show you how.
The Detail
Here’s the detail for those who want to understand more. If we look at the yearly proposed PFS rules over the last decade, there are three underlying themes that are part of a longer-term strategy. These are reflected in this year’s proposed rule as well. They are:
- Encouraging accountable care relationships (linking patients with responsible providers);
- Moving away from reliance of Traditional Medicare on FFS, and toward Accountable Care Organizations (ACOs) and Advanced Primary Care Management (APCM); and
- Shifting away from an emphasis on sick care to one that promotes prevention, chronic disease management and payment realignment
Let’s begin by taking a look at more details about the two provisions of the proposed rule that are uniquely transformative for population health: 1) the incorporation of an efficiency adjustment, and 2) the site of service payment differential.
Incorporation of an Efficiency Adjustment: For the first time ever, CMS is proposing incorporation of an
efficiency adjustment. This is a really important and overdue change and to fully appreciate it, let’s back up and take a look at how payment rates are set now for Traditional Medicare. Historically, CMS has leaned heavily on the American Medical Association’s Relative Value Scale Update Committee (RUC) to advise on payment values. The vast majority of RUC members are specialists and subspecialists and the preponderance of literature suggests that the result has been an overvaluing of procedural work and an undervaluing of cognitive work. The Primary Care Collaborative, National Partnership for Women and Children and others have written eloquently about the impact on primary care.
Starting in 2026, CMS is proposing an efficiency adjustment that would apply a 2.5% reduction to all codes except those at the heart of primary care, the time-based codes such as evaluation and management (E/M) services, care management services, behavioral health services and services on the Medicare telehealth list. If made final, this would set a fairer path going forward.
CMS anticipates that most specialties would see no more than a 1 percent change in total RVUs. Still, it is a good, policy-forward move overall no matter which side of the aisle you stand on.
Incorporating a Site of Service Payment Differential: For services performed in a facility setting, CMS would reduce the portion of indirect PE RVUs tied to work RVUs to half the amount used for non-facility services. Why is this important? In the current system, health systems have been acquiring physician practices in part to capture the differential additional payment that can be received under this structure.
In fact, a 2024 study in JAMA found that almost half of primary care providers are now affiliated with health systems and that the share of independent practitioners has decreased markedly over time.
Further, that when PCPs are acquired by health systems, in the current system they can be billed at a higher amount for the same service.
The end result would be to provide an immediate revenue boost for independent practices. Additionally, it is a start at stemming rising health care pricing associated with growing hospital ownership of primary care.
Likewise, MedPaC, suggests that as a “prudent purchaser,” Medicare should not pay more for the same service simply because it is delivered in a more expensive setting. CMS dipped a toe into the site neutral payment water in 2017 with limited site-neutral payment reform and key thought leaders like the Brookings Institution hailed the move as a “positive first step” noting that more needs to be done. The Kaiser Family Foundation 2025 report on Medicare site-neutral payment reforms as a policy lever echoes this sentiment. This year in the proposed 2026 PFS rule, CMS indeed takes a step forward with the change to the site of service differential.
If CMS Changes One Thing in the Proposed Rule, What Should It Be, and How Can I Make My Voice Heard to CMS?
If there were one modification to the proposed rule that would most benefit patients, from our perspective, hands-down, it would be waiving the cost-sharing for the Advanced Primary Care Management (APCM) Codes that were put in place by CMS beginning in 2025 and the new Add-On Behavioral Health Integration Codes introduced in the 2026 proposed rule. These are bundled payments that can be billed on a monthly basis to resource practices for providing a host of care coordination and management services so that they can operationalize team-based care. The problem is that they were a good idea in concept but are not well-utilized because they are hampered by the patient cost-sharing. It’s important to recognize that CMS has the authority to do this under current law, as ‘personalized prevention plan services’ can be provided without cost-sharing. This provides a viable basis for CMS to waive patient cost-sharing for the APCM codes and the new BHI add-on codes.
The proposed rule is open for comment until September 12th. If you want to register comments with CMS about the importance of waiving patient cost-sharing for the APCM and BHI add-on codes (or any other feedback or suggestions) to CMS for consideration in the final rule, it is easy to do. Comments must be submitted by September 12th . You may submit multiple comments as an individual and/or an organization and here is how:
- Go to Regulations.gov.
- Search for file code CMS-1832-P.
- Follow the “Submit a comment” instructions.
It is important to take the opportunity to comment as there will be many strong voices from those who benefit financially from the status quo who do not want to see change. Your voice counts. CMS takes the comment letters seriously and we have been heartened by the difference that comments have made in the past to make a good rule better.
The reconciliation package that was signed into law on the fourth of July, also known as H.R. 1 or the Big Beautiful Bill, has several impacts on health care but the largest by far is the imposition of Medicaid work requirements. H.R. 1 will reduce federal healthcare spending by $1.15T, though the Congressional Budget Office estimates that it will also increase the number of uninsured people by 11.8M by 2034.
It is important to gain an understanding of what will be required so that we can do our best as a community to help people understand, meet, and document so that they can retain coverage. It will require responsible and effective uses of technology, a comprehensive communication strategy, and a streamlined, user-friendly documentation and implementation system. States are required to implement the requirement by January 1, 2027, so it is important to get a head start now understanding what the law requires is a good first step.
Who Is Impacted?
The population of Medicaid members aged 19-64 who are covered through the Affordable Care Act Medicaid expansion or an 1115 demonstration waiver are the impacted group. Individuals in this group must (unless they fall into one of the exempted groups outlined below) demonstrate that they are engaged at least 20 hours a week, or 80 hours per month in employment, education, a work program, or community service to maintain their Medicaid eligibility.
It is important to note that there are many groups that are exempted from Medicaid Work Requirements, including:
- Individuals under age 19
- Pregnant individuals entitled to or enrolled in Medicare Part A or B benefits
- Foster youth
- Individuals enrolled in the Parents and Other Caretaker Relatives eligibility group
- Individuals eligible for a mandatory eligibility group
- Individuals recently incarcerated in the previous three months
- American Indians, Alaska Natives, and California Indians
- Parents, guardians, or caregivers of dependent children 13 years or younger or disabled individuals
- Veterans with total disability ratings
- Former foster care youth under age 26
- Medically frail individuals or those with special medical needs [as defined by the Secretary of the United States Department of Health and Human Services (HHS)], including:
- Blind or disabled individuals
- Individuals with a substance-use disorder
- Individuals with a disabling mental disorder
- Individuals with a physical, intellectual, or developmental disability that significantly impairs their ability to perform one or more activities of daily living
- Those with serious or complex medical conditions
- Individuals complying with Temporary Assistance for Needy Families (TANF) work requirements
- Members of a household that is in receipt of Supplemental Nutrition Assistance Program (SNAP) and not exempt from SNAP work requirements
- Individuals participating in a drug addiction or alcohol treatment and rehabilitation program
- Inmates of public institutions
- Pregnant individuals or those receiving postpartum coverage
It is also possible that states may allow exemptions for extenuating circumstances, including
individuals receiving care in hospitals, nursing facilities, psychiatric facilities, or other intensive care
settings, individuals in a federally declared disaster area, individuals living in counties with
unemployment rates higher than eight percent, or 1.5 times the national unemployment rate (pending
permission from HHS secretary), and individuals or their dependents who are required to travel outside their home for medical care for an extended time.
What Are the Timelines?
In general, states are required to communicate to impacted beneficiaries in at least two modalities between June and September 2026. Full implementation of the requirements will begin by December 31, 2026. Timing may vary slightly as states may appeal to the federal government for adjustments to the requirements.
Are There Helpful Resources Available?
The Center for Health Care Strategies has created a helpful and concise tool (A Summary of National Medicaid Work Requirements) that captures the essentials and may be helpful to share with your team members. As well, the Kaiser Family Foundation has prepared a helpful explainer that provides a closer look at the requirements.
It’s no secret that primary care is the keystone of effective, efficient care delivery. The primary care workforce is the beating heart of the system and a number of recent publications have shed additional light on how it is changing over time. The National Center for Health Workforce Analysis published The State of the Primary Care Workforce which calls additional attention to the need to build up the primary
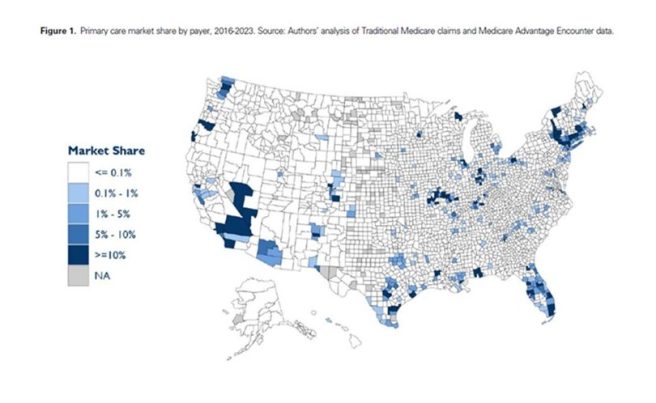
care workforce nationally. In addition, Adler, Crow, et. al. published a wonderful piece in the June 11th edition of Health Affairs Scholar that sheds light on payer-primary care integration. They use data through 2023 so it is possible that their estimates may be understated. They find that payer-operated practices account for 4.2% of the national primary care market by service volume in 2023, up from 0.78% in 2016. It’s not clear yet what the implications will be from these arrangements in the long term, but it is interesting to see how the magnitude of payer-owned practices is concentrated largely in select regions of the nation. The authors note a direct relationship of more payer-owned practices in regions with higher Medicare Advantage penetration.
The authors include an interesting geographic representation of the magnitude of payer ownership of primary care practices throughout the nation. For Michigan, the regions with concentration are in Marquette, southeast Michigan, and Grand Rapids. For an additional perspective on payer ownership of primary care practices in the Midwest, consider that there are no counties in Michigan where payer-owned primary care represents 10% or more of the primary care market, but one county in Ohio (Summit) and one in Illinois (Cook) do. Take a look at how rates compare across the country:
We take a moment to pause to reflect on the legacy of Lucian Leape, MD, considered by many to be the father of the patient safety movement, who passed away this summer. You might remember that Dr. Leape for his thoughtful and laborious review of medical records of hospitalized patients that identified both things gone right and things gone wrong in their care and that substantiated the need to address iatrogenic and nosocomial infections as well as lack of attention to process. He was decried at first by the medical establishment and then embraced as a visionary. As a member of the Institute of Medicine’s (now the National Academy of Medicine’s) Quality of Care in America Committee, he was influential in both their “To Err Is Human” and “Crossing the Quality Chasm” reports.
His seminal work was the Medical Practice Study which found that two-thirds of the injuries to patients were caused by errors that appeared to be preventable. He was once asked about one thing he’d like to change about healthcare and he responded “the payment system”. He believed in a salaried model for physicians that could ease the production pressure on them to see more patients in less time rather than focus on the quality of their interactions with patients. It’s food for thought as we strive to deliver on the quintuple aim.
Honoring Hae Mi Choe’s Legacy

We are saddened to share the news of Dr. Hae Mi Choe’s passing in July after a courageous battle with an aggressive form of leukemia. Dr. Choe will be remembered for many things, including her pivotal work in Michigan linking community pharmacists with primary care providers and patients to ensure that patients had an understanding of their medications, an ability to have their questions answered, and their PCPs kept in the loop as partners in operationalizing team-based care.
Read along with the Primary Care Review community! We’ve combed the recently published literature to choose a few select morsels worth your time. We hope you’ll agree!
This month, we spotlight two articles from the Journal of General Internal Medicine that focus on straightforward, actionable ideas for change to enhance primary care clinic portal message workflow efficiency.
- Taming the In‑Basket—How Two Simple Tools Reduced Portal Message Volume in an Academic Internal Medicine Clinic, by Nicole Hadeed, MD and colleagues; and
- Surprisingly Helpful: The Introduction of Portal Practice Slots to Address the In-basket Explosion,” by Jennifer Reilly Lukela MD, et. al.,
Hats off to the authors (from Michigan Medicine) who do a nice job testing and refining two helpful interventions. The first publication identifies targeted interventions that can reduce portal message burden and improve workflow efficiency in primary care through standardized protocols and role clarification. The second highlights the importance of incorporating protected slots in a provider’s schedule. The ideas as applicable for consideration in an academic medical center as at an independent provider’s office.




