Primary Care Review – Summer – July 2025
A Deep Dive into HHS and CMS New Strategies
Over the last month and a half, HHS and CMS have released a good deal of information that provides insight into what we can expect to see in priorities and programming over time. Though each released document focuses on a slice of the CMS and HHS portfolios, four key overarching themes look to be woven throughout:
- Unleashing Technology
- Ensuring Shared Risk and Skin in the Game
- Prioritizing Financial Stewardship, and
- Being Open to New Ideas and Change
Let’s take a look at each of released documents with an eye toward impacts on primary care and population health.
1. New CMS Innovation Center Strategy
The new CMS Innovation Center (or Center for Medicare and Medicaid Innovation, CMMI) white paper and accompanying FAQ were released on May 13, 2025. They focus on three central pillars:
a. Promoting evidence-based prevention
All three levels (primary, secondary, and tertiary) of prevention are addressed with an openness to community-based initiatives. There is a lot for primary care and population health to like about this focus, particularly the idea of new ways to support the initiation and maintenance of constructive lifestyle changes (e.g., exercise, nutrition, etc.) including the potential for beneficiary incentives, and partnering with community-based organizations. The success of Accountable Care Organizations (particularly those led by primary care physicians) in moderating cost, attending to prevention, and producing outcomes is worth reflecting upon here.
b. Empowering people to achieve their health goals
This includes helping people get user-friendly information that is easily available when they need it, as well as encouraging people to partner in their care and make informed decisions that are right for them. In addition to increasing patient access to data and to comparative provider performance, the white paper specifically lists the examples of mobile devices, apps shared decision-making tools, and health education materials.
c. Driving choice and competition for people
As a health system become more consolidated and purchase or merge with smaller systems and/or purchases primary and specialty care practices, they are able to exercise increased negotiating power (https://www.rand.org/pubs/research_reports/RRA1820-1.html ). In addition, when primary care practices are acquired and provided in hospital outpatient facilities, a separate fee can be charged in addition to the underlying service. Commercial insurers and patients feel the cost increases, and so does CMS. Bolstering independent practice provides a counterweight to the increase in consolidation and may be helpful in ensuring that beneficiaries and patients who live in rural and underserved locations have access to care as well. In addition,
New models will be built with a concerted aim to, when completed, be able to satisfy the actuarial requirement for certification. Thus, that an idea will achieve cost savings will be key. To reduce the selection bias and catalyze change, it is possible that the Center may require participation for some endeavors.
2. New Report on Childhood Chronic Disease
The Make America Healthy Again (MAHA) Report on Childhood Chronic Disease was originally issued on May 22, 2025 and pulled back by Administration, but reissued shortly afterward in its current form. The reissued document corrects some citation and study reference issues in the original report. The report is a product of a Presidential Commission to focus on building a healthier America and an accompanying strategy is expected to be released in mid-August.
The report focuses on the higher-than-desirable percent of children with chronic disease and points to four major contributing factors: 1) poor diet, 2) exposure to environmental toxins, 3) lack of physical activity and chronic stress, and 4) overmedicalization. Even with the corrected citations, the report remains somewhat controversial in some of its claims, especially in light of the substantial literature supporting vaccine safety.
However, many recommendations resound across a wide variety of audiences, including:
- Requiring nutrition courses in medical school curriculums;
- The influence of corporate interests in policy setting; and
- The need to increased attention and interventions to address the issues of nutrition, lifestyle, and exposure to pollution and harmful chemicals.
3. CMS National Quality Strategy
Early June was a busy time for health technology and information policy at the federal level. With the recent appointment on June 3rd of Dr. Thomas Keane as Assistant Secretary for Technology Policy (ASTP) and National Coordinator of Health Information Technology, the stage is set for additional policy to be announced. He comes with experience at the federal level and a background as both a physician and a software engineer. As Dr. Keane steps into his role, the agency is reviewing a host of submissions to a Request for Information (RFI) on the Health Technology Ecosystem that was issued in May.
The same day that Dr. Keane’s appointment was announced, so were several initiatives including:
- Building a dynamic, interoperable national provider directory;
- Bringing modern identity verification processes to Medicare.gov to streamline credentials across the healthcare system;
- Expanding functionality of CMS’ Blue Button 2.0 patient access application programming interface (API);
- Transitioning CMS’s Data at the Point of Care pilot to general availability; and
- Enhancing CMS’ participation in trusted data exchange
The CMS National Quality Strategy is evolving, and we anticipate additional information about direction to come out soon. This said, reduction of administrative burden in the collection of data and improving the sophistication of analysis as well as increasing the usefulness of reporting will continue to be important. Importantly, the Universal Foundation, a set of streamlined adult and pediatric measures, has been echoed identified as being key to a healthier America, as have Meaningful Measures 2.0
We also anticipate high priority on moving to digital quality measures and an increased focus on person-reported outcome performance measures. In addition, there is likely to be a continuing focus on:
- Outcomes and Alignment
- Access for All and Engagement
- Safety and Resiliency
- Interoperability and Scientific Advancement
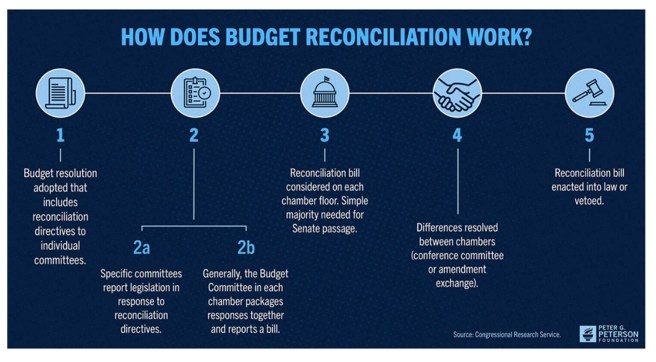
A Word About What’s Going on in DC
As this issue goes to press, the process of budget reconciliation is playing out in our nation’s capital. The final outcome will have implications on important issues like Medicaid, the ACA Marketplace, and access. As a backdrop to better understand the process, the federal government’s fiscal year runs from October 1st to September 30th, and it is always preferable to have things wrapped up by the end of September to avoid the potential of a “government shutdown,” but the actual timing of a final bill is unclear. It is possible and even likely that there will be resolution before the GOP’s self-imposed July 4rth timeline. On the other hand, one can never rule out a surprise externality.
Though the President plays a role in submitting a proposal, it is ultimately Congress who must iron things out and approve a final budget. At this point, the House bill has crossed over to the Senate where it was further amended. There are special rules that apply that are meant to streamline reconciliation. Passage requires only a simple majority (not three-fifths) of the Senate. Filibustering is also prohibited in the Senate for reconciliation and changes introduced can only if they impact budgetary provisions.
The resulting Senate language is sent back to the House (that’s where things stand now) where it will be voted on again. As the bill can only be sent to the President for signature or veto after the House and Senate adopt the same version.
Three cheers to the Peterson Foundation who created a lovely infographic that visualizes the process:
Site Neutral Payment Policy
As health system consolidation increases in Michigan and nationally, its impact on pricing is much in the news as is the idea of site neutral payment. With site neutral reimbursement, payers (usually starting with Medicare) pay the same rate for the same service, whether it is provided in a hospital outpatient department (HOPD), ambulatory surgical center (ASC), or freestanding physician office. Now, Medicare pays hospital outpatient departments higher rates than freestanding ambulatory surgical centers and physician offices for providing similar health services. This difference in payment across settings for the same service has created a financial incentive for hospitals to acquire physician practices and other entities.
MedPAC, the independent, non-partisan legislative branch agency that advises the U.S. Congress on the Medicare program, has supported implementation of site-neutral payment since its 2023 report to Congress and recommended that payments be aligned across HOPDs, both on-campus and off, ASCs and physician offices for certain ambulatory payment classification (APC) groups.
Site neutral payment was introduced in a limited way in the Bipartisan Budget Act of 2015 with a wide range of exceptions, but a recent analysis by Post, et. al., (10.1377/hlthaff.2024.00972
HEALTH AFFAIRS 44) NO. 6 (2025): 659–667) found that there were so many exceptions that “the act did little to reduce Medicare spending or hospital-physician integration, suggesting that site-neutral legislation could be strengthened by reducing exceptions.” Hospital and health systems have traditionally opposed expanding site neutral policy and express concern about implications for patients.
However, a recent study by Lou, et. al. (10.1377/hlthaff.2024.01501 HEALTH AFFAIRS 44, NO. 6 (2025): 668–676) thoughtfully assesses the impact of broadening the extent of site level payment and finds that small and rural hospital would absorb the smallest share of cuts and that “site-neutral payments would not have substantially different effects on beneficiary groups defined by dual-eligibility status or age”. Lou and colleagues suggest a nuanced way to implement expanded site neutral policy that protects against undue adverse effects. It is a publication worth a second and third reading as the nation searches for policy solutions.
CMS Announces Adjustments to ACO REACH for 2026
ACO REACH has been an interesting program for many reasons, chiefly because it aligns incentives among many different kinds of providers including primary and specialty care physicians. Additionally, primary care-led ACOs tend to outperform others given their focus on team-based, coordinated care.
Over time, it is not unusual to see the bar raised as organizations gain experience with value-based approaches. In this vein, CMS has announced changes for the 2026 performance year to “improve model sustainability” including:
- Increasing the portion of benchmark that is historical (as contrasted with regional) to 60%
- Adding a 3% cap on risk score growth from 2019 to 2026 (quality withhold goes from 2% to 5%)
- Boosting the coding intensity factor ceiling for high-needs ACOs from 1% to 2%
The ACO Reach demonstration is scheduled to end on December 31, 2026, and some think that the changes improve the likelihood that the program will be extended.
Medicare Diabetes Prevention Program (MDPP) Evaluation: Facilitating Successful Lifestyle Change
The final evaluation report of the Medicare Diabetes Prevention Program (MDPP) Expanded Model was recently released and the results were very impressive. Though it enrolled far fewer beneficiaries than optimal, the program combined classes with coaching, and produced an average weight loss per participant of 4.9%. Given the challenge of achieving lifestyle change toward healthier behaviors, the report is something to both celebrate and learn from.
July 8th Obesity Measurement CMS Webinar
Obesity and interventions to stem it have always held a place of importance, but CMS has signaled an interest in moving toward the use of weight management intervention outcome, not just process measures like screening and counseling. It may also be an opportunity to learn more about the transition to digital quality measures for obesity. To attend the July 8th 1PM ET webinar, register at the Zoom for Government site.
Now Available: 2025 MMI Comparative Collaborative Care and Telehealth Payer Policy Tables
We are grateful to the Payer Leader partners across the state without whom, we could not have prepared the 2025 update of the Collaborative Care and Telehealth comparative payer policy tables. You will find that there are several places where payers approach alignment on policy, and others where the variation among payers is greater. In either case (though we are big fans of aligned, evidence-based policy) the comparative payer policy tables serve as a useful comparison and high-level overview of how policies compare, though they are not a substitute for detailed payer billing and coding requirements.
Unhurried Conversations in Health Care
The Dawna Ballard and colleagues take on the importance of ensuring the time for unhurried conversations, and confronts the challenges of life on the frontline of primary care. The article can be found at: Unhurried Conversations in Health Care Are More Important Than Ever: Identifying Key Communication Practices for Careful and Kind Care | Annals of Family Medicine. Victor Montori, MD from Mayo serves as senior author and the article underscores his commitment to “careful and kind care”.
Importantly, the authors provide recommendations for how to make practice and incremental change now. The authors outline ten microlevel communication practices that support an unhurried conversation with implementation suggestions, including shared turn-taking, strategic use of pauses, and triaging topics.
Whole Person Health
In How Are You Doing… Really? A Review of Whole Person Health Assessments , Gold and colleagues, including Rebecca Etz, author of the Person-Centered Primary Care Measure (PCPCM) examine the field of whole person health, a person-centered, integrated approach to care that focuses on health and well-being by incorporating patient’s goals for their own health.
They identified four overarching categories of whole person health, consisting of nine domains: body and mind (physical well-being, mental/emotional well-being, meaning and purpose [spiritual well-being], sexual well-being), relationships (social well-being), living environment and finances (financial well-being, environmental well-being), and engagement in daily life (autonomy and functioning, activities).
Whole person health assessments are consistent with a biopsychosocial construct to partnering with patients, and a promising approach that underscores moving beyond a sick care focus to one that is upstream, holistic, and reflective of the things that matter to patients.

