
There is a statue of Albert Einstein in front of the National Academies of Sciences building in Washington DC. On the base of the status is a quotation by Einstein, a member of the Academies, that says “The right to search for truth implies also a duty; one must not conceal any part of what one has recognized to be true.”
One thing that has been well-recognized to be true is that primary care is the underpinning of a well-functioning health system. The National Academies of Sciences, Engineering, and Medicine (NASEM) landmark 2021 report, Implementing High-Quality Primary Care identified a listing of policy changes that are needed if we are serious about strengthening primary care. Hats off to CMS leadership for doing the hard work of starting to incorporate the NASEM guidance on evolving primary care reimbursement toward hybrid primary care payment. In the proposed 2025 Physician Fee Schedule, CMS introduces three proposed new Advanced Primary Care Management codes (APCM)– a big step toward hybrid payment reform for Medicare FFS.
Let’s look at the requirements for the proposed new codes:
- Patient Consent: Inform the patient about the service, obtain consent, and document it in the medical record.
- Initiating Visit: For new patients or those not seen within three years.
- 24/7 Access: Provide patients with urgent care access to the care team/practitioner at all times.
- Continuity of Care: Ensure continuity with a designated team member for successive routine appointments.
- Alternative Care Delivery: Offer care through methods beyond traditional office visits, such as home visits and extended hours.
- Comprehensive Care Management:
- Conduct systematic needs assessments.
- Ensure receipt of preventive services.
- Manage medication reconciliation and oversight of self-management.
- Electronic Care Plan: Develop and maintain a comprehensive care plan accessible to the care team and patient.
- Care Transitions Coordination: Facilitate transitions between healthcare settings and providers, ensuring timely follow-up communication.
- Ongoing Communication: Coordinate with various service providers and document communications about the patient’s needs and preferences.
- Enhanced Communication Methods: Enable communication through secure messaging, email, patient portals, and other digital means.
- Population Data Analysis: Identify care gaps and offer additional interventions.
- Risk Stratification: Use data to identify and target services to high-risk patients.
- Performance Measurement: Assess quality of care, total cost of care, and use of Certified EHR Technology.
These thirteen requirements are very similar to the activities expected of Michigan’s over 300 CPC+ practices and reflective of expectations already in place by several Michigan payers. Many primary care practices in Michigan already operationalize these requirements, and that is a good thing, making the new codes for Medicare FFS even more attractive to many practices in the Great Lakes state.
The new codes also fill a need that practices have long asked for – stable, expected funding for care management activities. Practices tell us again and again that the thing that they most appreciated in primary care demonstrations like the MiPCT and CPC+ was the monthly advanced primary care management fee. The new APCM codes are built on that platform and function similarly. They don’t require time-tracking and can be billed across the array of Medicare FFS patients, from those who have no chronic disease to those who are multimorbid. It’s also possible and often the case that commercial, Medicaid, and Medicare Advantage plans adopt the new codes that CMS puts in place for Medicare Traditional FFS.
Here is a glimpse of the structure of the new codes: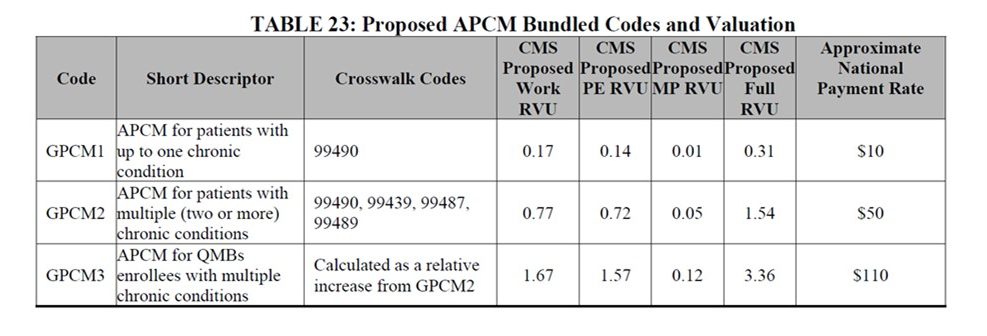
The APCM codes mean that practices that meet the requirements can receive payment (one of three levels, depending on a patient’s complexity) to manage population health and coordinate patient care. The new APCM codes also help to prepare practices for the shift away from fee-for-service payment toward value-based care and payment. No codes are perfect and some patients without Medigap (about 10%) may face a 20% cost share. Still, the new codes represent a major step forward for implementing hybrid payment in advanced primary care. CMS should be applauded for taking a big step forward for all of primary care.
