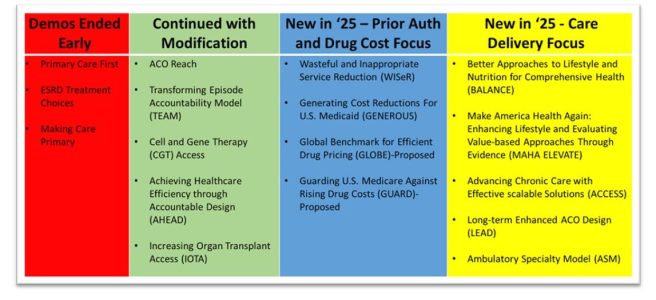
2025 was a busy year for the Center for Medicare and Medicaid Innovation (CMMI), the agency within CMS that develops and tests promising new healthcare payment and service delivery models for their ability to improve quality, reduce unnecessary cost, and improve patient experience. CMMI ended some demonstrations early, modified components of other demonstrations, and launched an array of new demonstrations – ten in the past two months alone. Some of these new demonstrations focus on prior authorization and drug pricing, but of special focus to those interested in primary care and population health are those rooted in care delivery.
Taken as a whole, it appears that CMMI is signaling interest in making sure that model designs will produce their intended end goals such as cost savings. And as we’ve seen across administrations, the commitment to value-based payment and beneficiaries in accountable patient and clinician relationships is here to stay. So is aligning financial incentives so that multiple healthcare partners who are caring for a beneficiary provide efficient, effective care throughout a beneficiary’s care journey. There is also an intentional focus on chronic disease prevention and management focus woven into expectations and approaches.
Let’s take at each of the new care delivery-focused models (BALANCE, MAHA Elevate, ACCESS, LEAD, and the ASM) with a focus on how each impacts primary care and population health. Note that CMMI has yet to release additional details and application material for some of the models. Still, it is helpful to understand the basic parameters of each new model to gauge their applicability and interest in your work serving patients.
- Better Approaches to Lifestyle and Nutrition for Comprehensive Health (BALANCE) aims to increase access to select GLP-1 medications and healthy lifestyle interventions for Medicare and Medicaid beneficiaries through CMS drug pricing negotiation on behalf of state Medicaid agencies and Medicare Part D plan sponsors. The intent is to make anti-obesity medications more affordable as a treatment option when appropriate. The program is expected to launch in 2027 with an early bridge component to the demonstration kicking off in mid-2026.
| BALANCE DEMO ROLE FOR PRIMARY CARE: No direct role or opportunity to participate in the demonstration, per se. The BALANCE demonstration and other initiatives may result in decreased pricing of GLP-1 medications for some patients. As well, all beneficiaries receiving GLP-1s for weight management under BALANCE are to be provided access to a lifestyle support program by the manufacturer at no cost. The lifestyle intervention is intended to offer education on how to maintain weight loss and make positive health choices to help improve health. |
- MAHA Enhancing Lifestyle & Evaluating Value-based Approaches Through Evidence (ELEVATE) Elevate is a three-year program aimed at reducing chronic disease progression by funding evidence-based functional and lifestyle medicine approaches, such as nutritional support and physical activity not covered by Original Medicare. Private practices, health systems, ACOs, academic organizations, community-based organizations and others will be eligible to submit an application detailing their proposed approach and approximately thirty awards will be made with a composite total of $100 million and a start date of September 2026.
| MAHA ELEVATE DEMO ROLE FOR PRIMARY CARE: No direct role unless you are affiliated with a larger organization that receives an award. Such practices may have the opportunity to support intervention implementation integration in patient care. |
- Advancing Chronic Care with Effective Scalable Solutions (ACCESS) is focused on reducing payment barriers to digital health tool use. On one hand, it is important to adapt to new innovations in patient self-management support and remote monitoring. On the other, for the many new tools that are emerging, it is sometimes difficult to discern between hype and demonstrated ability to support patient self-management of chronic disease.
ACCESS is a ten-year national voluntary demonstration of technology-supported care for early and late cardiometabolic and kidney conditions, musculoskeletal conditions, and behavioral health conditions, including depression or anxiety. There are expected to be outcomes-aligned payments from CMS to the selected technology vendors as well as some payment to the providers who are supporting patients using approved technologies in the demonstration.
Nationally, several payers have also signed up to align with the core concepts of the ACCESS model. So far, Arkansas Blue Cross and Blue Shield, Blue Shield of California, Blue Cross and Blue Shield of Minnesota, Blue Cross Blue Shield of North Dakota, BlueCross BlueShield of Tennessee, CareFirst BlueCross BlueShield, Centene, Cigna, CVS Health, Devoted Health, Guidewell, Horizon Blue Cross Blue Shield of NJ, Humana, and UnitedHealthcare have indicated that they will do so. Though there are no Michigan-based payers in this set as of yet, adoption by multiple payers should help to reduce administrative burden and build volumes for scalable implementations. The ACCESS model includes a reporting infrastructure that incorporates a new health information standard called Fast Health Interoperable Reporting (FHIR). This means that not only is the demonstration a test of technology-supported care, it is also a test of interoperability feasibility and readiness in real-time. The model has a ten-year span with a start date of July 5, 2026.
| ACCESS DEMO ROLE FOR PRIMARY CARE: CMS will maintain a public directory of digital health tools approved in the ACCESS demonstration. Primary care practitioners will be able to refer patients, though patients will also be able to sign up directly with participating ACCESS organizations. Primary care clinicians will be able to bill a co-management payment to CMS (and potentially to other participating payers) for reviewing electronic updates and documenting related care coordination activities (e.g., medication adjustments, etc.) for ACCESS patients in the demonstration when they take an active role in oversight and coordination. |
- Long-term Enhanced ACO Design (LEAD) is the long-awaited successor to ACO Reach. In LEAD, CMMI has worked to make ACO participation more feasible for smaller, independent providers and organizations serving underserved or complex populations. It is a ten-year voluntary model open to current ACO REACH participants, Medicare FFS providers who are new to accountable care, providers serving underserved populations including dual eligibles, Federally Qualified Health Centers (FQHCs) and Rural Health Centers (RHCs) as well.
There are two kinds of participants in LEAD: Participant Providers and Preferred Providers. Physicians and health care organizations that elect to be Participant Providers take direct accountability for cost and quality and drive beneficiary alignment. LEAD will use a whole Tax Identification Number (TIN) approach, which captures all National Provider Identifiers (NPIs) billing under a Participant TIN as Participant Providers.
Preferred Providers, on the other hand, take indirect financial accountability and do not drive beneficiary alignment or quality performance for the ACO, per se. For example, specialists and institutional providers (e.g., post-acute care) might be particularly drawn to Preferred Provider participation. Preferred Providers will be managed at the TIN-NPI level, with the intent of providing Participant Providers more specificity and flexibility in partnerships.
LEAD participants select one of two levels of risk-sharing: 1) Global risk with 100% upside or downside risk relative to the established performance benchmark, or 2) Professional risk with 50/50 gain or risk sharing depending on performance. There are a few design components in LEAD that make it especially interesting. For example, LEAD is designed with a goal of increasing stability in benchmarks. Unlike REACH ACO, LEAD will not have annual rebasing. In addition, the model offers the opportunity for beneficiary enhancements and incentives to encourage patient engagement.
In an attempt to reduce the complexity of building the entire array of partnerships necessary to care for ACO patients, CMS introduces CMS Administered Risk Arrangements (CARAs) that are intended to provide support to ACOs to enable episode-based risk arrangements between ACOs and their specialists and provider organizations to facilitate greater and stronger Preferred Provider relationships with these downstream health care providers. In these structures, CMS administers the arrangements and facilitates information sharing.
This will include common contracting frameworks by enabling export of episode information into contracting templates. These voluntary components facilitate digital data-sharing and payment among preferred providers, downstream specialists and provider organizations. CMS could then share episode data with ACOs and the Preferred Providers with whom they enter into episode-based risk arrangements (EBRAs).
LEAD not only extends the traditional time frame for demonstrations as it has a ten-year lifespan, but it also extends a bit beyond the Traditional Medicare population by working with two selected states to include Medicaid beneficiaries. CMS also tries to more fully adjust for the work involved in managing the care of complex patients. A comparison and contrast between ACO Reach and LEAD is shown below:
ACO Reach and LEAD ACO Comparison

Applications for LEAD participation are not out yet but expected to be released soon, as the application period opens in March 2026 with a model launch date of January 2027.
| LEAD ROLE FOR PRIMARY CARE: If you participated in REACH ACO or are new to accountable care, treat underserved populations including dual eligibles, are a Federally Qualified Health Center (FQHC) or Rural Health Center (RHC), you may want to explore LEAD as a gateway to increase your experience with value-based, accountable care. Given the way that CMS has decreased barriers to entry for smaller providers and those that serve high-needs populations, for those new to accountable care two-sided risk arrangements, it may be hard to find a better opportunity to test the ACO waters. In either case, modeling the financial impacts when additional details and the demonstration are released at the LEAD website will be a good place to start. |
- The Ambulatory Specialty Model (ASM) reflects CMMI’s extension of two-sided risk beyond primary care and Accountable Care Organizations and into specialty outpatient care. Though the model is specialist-focused, participating specialists are required to establish Collaborative Care Arrangements (CCAs) with primary care providers to define shared roles, data-exchange expectations, and joint responsibility for patient management, including transitions between care settings.
The ASM is a two-sided risk payment model that will be mandatory in selected Core-Based Statistical Areas (CBSAs) for specialists who commonly treat Medicare beneficiaries for heart failure or low back pain in outpatient settings. In Michigan, the selected ASM areas will be: Flint, Jackson, Kalamazoo-Portage, Midland, Owosso, Saginaw, Traverse City, and Warren-Troy-Farmington Hills. The other ASM regions shown below on the map are fairly well-distributed nationally.
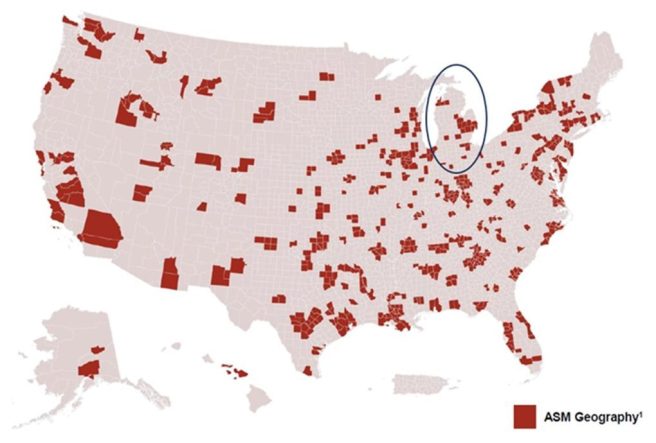
The ASM aims to improve prevention and upstream management of chronic disease and is intended to produce reductions in avoidable hospitalizations and unnecessary procedures. Payment is based on performance relative to their peers which will determine the payment adjustment on their future Medicare Part B claims for covered services.
The model will begin on January 1, 2027 and run for five performance years through December 31, 2031. Many think that it is likely that over time, CMMI may add more conditions and specialties into the model design.
| ASM ROLE FOR PRIMARY CARE: Though model participants are specialists who treat patients with heart failure and low back pain, these providers will be required to establish a formal relationship with at least one PCP. This allows for tighter integration between PCPs and specialists in the management of specific, high-cost, high-volume conditions. |
